Writing cross-published from Medium
Antibiotic resistance is an emerging major problem that has already become a threat to public health, as acknowledged by the WHO. It is part of the consequences of countless years of healthcare misconduct, allowing earlier antibiotics like penicillin to be circulated in the market and be freely used without concerning the possibility of a resistance. Throughout those years, countless of bacteria that showed no significant opposition towards antibiotics gradually started to find its way around the specific toxicity by acquiring resistance towards them.
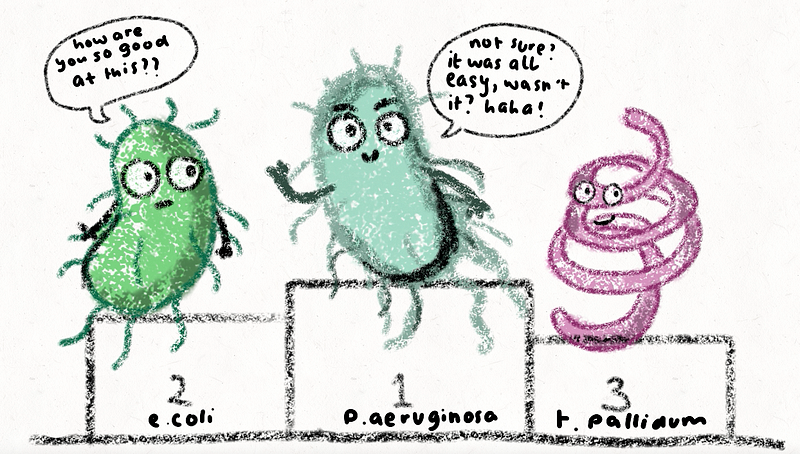
But the thing is, the Pseudomonas aeruginosa didn't need all these 'years of planning' to become resistent. They have always been good at what they do, on top of the class, best at resisting any type of antibiotic that is in store for them, without needing external intimidation or an adapted gene mutation. That can be seen by how earlier bactericidal antibiotics, like antipseudomonal penicillin and cephalosporin, have specific categories made just to eliminate this tough guy. Just like how some students are in school, intelligence cannot be judged by the amount of studying they do, some are just… naturally gifted? and Pseudomonas aeruginosa can be considered one of those annoyingly smart, no effort students. They already have a survival instinct of their own, allowing them to bypass antibiotic mechanisms, without needing multiple earlier exposure to the drug. But how does this happen?
this is the type of resistance that isobtained without possessing earlier activity against the antibiotic, and that it does not involve any transfer of genetic material. This means that even from the start, like inheriting intelligence from parents, Pseudomonas aeruginosa have already had the upper hand; privileged with special abilities that made them naturally insusceptible to antibiotics.
To deactivate antibiotics, the most straightforward thing to do is to cut through the structure, and Pseudomonas aeruginosa hold the scissors.
Proteins can be made into a lot of things, much to the cell's liking. One of the most prominent things that is mainly made out of protein are enzymes, that acts as biological catalysts by accelerating chemical reactions. Adding to the list of Pseudomonas aeruginosa's natural intelligence, the species have been attired with a specific enzyme that can cleave several structures of an antibiotic, specifically ones that has the beta-lactam ring.
If you haven't heard of the beta-lactams yet, that means that you've probably have lived under a rock in the bacteria world, because the beta-lactam family are probably one of the earliest, most exploited (heavily exposed to antibacterial resistance) antibiotic that has introduced a whole lot of 'prominent names', such as amoxicillin and ertapenem. The beta-lactam have a common trait to affect the synthesis of the cell wall structure, and are still widely used to this day.
Beta-lactams can be cleaved by… you guessed it, the beta-lactamase, a specific restricting enzyme that can be found in normal Pseudomonas aeruginosa. They typically carry around the AmpC gene, a conventional beta-lactamase that conveys resistance to penicillin and earlier generations of cephalosporin. The AmpC gene works by breaking the amide bond of the beta-lactam ring, leading to deactivation.
Another one of the Pseudomonas aeruginosa's special traits is the ability to not only cut a backbone structure of the antibiotic, it can also induce structural conformation. An example to this is another huge, renowned family with a 'micin' surname, the aminoglycosides, that can be modified by enzymes such as the aminoglycoside phosphotransferase (APH), aminoglycoside acetyltransferase (AAC) and aminoglycoside nucleotidyltransferase (ANT). From the 'transfer' in its name, it's pretty self-explanatory that its focus is to "transfer things", but in this case is "transferring things to stir chaos". The APH in Pseudomonas aeruginosa will transfer the phosphoryl group from one point to another, which again, deactivates the antibiotic from its effective state.
Pseudomonas aeruginosa never fails to cut off from the things that are toxic for them, and they throw it all to the trash.
Think of efflux pumps as a microorganism's garbage chute, where they throw out all the things they don't need and/or think is dangerous. Unless they are masochists, it's obvious that bacteria wouldn't want to have antibacterial components to stay inside their system, and the same thing goes to the all-mighty Pseudomonas aeruginosa. Efflux pumps removes a huge range of residues, such as organic solvent, detergents, fatty acids, toxic lipids and quorum sensing molecules.
There are five types of efflux pumps, but the one that is associated with the Pseudomonas aeruginosa is the resistance-nodulation-division (RND) family, that is widespread among gram-negative bacteria.
The RND will capture a number of substrates from the cytoplasm, the leaflet of the inner membrane, and the periplasm, supported by a three-part (tripartite) protein complex that can expel the substrates through a channel protein.
the mechanism of RND efflux pump, expelling substrates (including antibiotics) out of the cell, from the inner, outer, and periplasmic membrane.
It is hard to introduce yourself into a Pseudomonas aeruginosa's life… because they usually keep their doors sealed shut.
Cell membrane penetration is a critical point to insure Pseudomonas aeruginosa's susceptibility to antibiotic. But just like the other aspects mentioned, Pseudomonas aeruginosa is quite different than the others.. one might even say, rather hostile to new elementals.
The outer membrane of Pseudomonas aeruginosa is completely restricted, with permeability as low as 8% of that of E coli. Pseudomonas aeruginosa, just like any other gram negative bacteria, has an asymmetric bilayer of phospholipid, and in this structure are integral membrane proteins called porins that facilitates transport in and out of the cell, generally through diffusion.
There are a lot of types of porin, but the most predominant porin in Pseudomonas aeruginosa are the OprF, which are responsible for non-specific intake of ions and saccharides, but awful at antibiotic permeation (and for a good reason). Not only that, most OprF porins don't even form open channels, only 5% of them do, which is absolutely misleading, to say the least. A quite effective porin that exists in Pseudomonas aeruginosa and is most commonly targeted for antibiotic permeation are the OprD, but even those openings are starting to be inaccessible due to emerging acquired resistance.
the pseudomonas aeruginosa OprF porin, not letting in any unknown substrates into the cell.Pseudomonas is ambitious and strives to be the best in all sectors; straight As, Class President, acceptance letter to Harvaid. Because of that, it studies and studies hard, probably harder than you. It gains extrinsic resistance, whether it be from intrinsic gene mutation or receiving resisting genes from another, creating another strain of super mutant variants, or a more general (but less cooler) general term of that would be multidrug resistant strains.
With the Pseudomonas aeruginosa getting stronger and stronger, and conventional antibiotics starting to lose its effect, scientists are on the run to beat Pseudomonas in its own game, through novel therapeutic strategies (and a special article will be posted regarding that, so stay tuned!). The best we can do now to combat these dangerous tiny beings is of course, to regulate the use of antibiotics and use them as instructed, and only as it's instructed.
Because to defeat the Pseudomonas aeruginosa in class, you should prove yourself to be smarter than they are.
References:
https://www.bfr.bund.de/en/questions_and_answers_on_esbl_and_ampc_producing_antimicrobial_resistant_bacteria-132522.html. accessed on 28 October 2023, 11.27.
Alenazy, Rawaf. 2022. "Drug Efflux Pump Inhibitors: A Promising Approach to Counter Multidrug Resistance in Gram-Negative Pathogens by Targeting AcrB Protein from AcrAB-TolC Multidrug Efflux Pump from Escherichia coli" Biology 11, no. 9: 1328. https://doi.org/10.3390/biology11091328
Housseini B Issa, K., Phan, G., & Broutin, I. (2018). Functional Mechanism of the Efflux Pumps Transcription Regulators From Pseudomonas aeruginosa Based on 3D Structures. Frontiers in molecular biosciences, 5, 57. https://doi.org/10.3389/fmolb.2018.00057
Poole K. (2011). Pseudomonas aeruginosa: resistance to the max. Frontiers in microbiology, 2, 65. https://doi.org/10.3389/fmicb.2011.00065
Zheng Pang, Renee Raudonis, Bernard R. Glick, Tong-Jun Lin, Zhenyu Cheng, (2019). Antibiotic resistance in Pseudomonas aeruginosa: mechanisms and alternative therapeutic strategies. Biotechnology Advances, Volume 37, Issue 1.